Abstract
There is growing interest in N-desmethylclozapine (NDMC), the major metabolite of clozapine, as a unique antipsychotic because it acts in vitro as a 5-HT2 antagonist and as a partial agonist to dopamine D2 and muscarinic receptors. To explore this, we compared NDMC to a typical (haloperidol), atypical (clozapine), and partial-agonist atypical (aripiprazole) antipsychotic in preclinical models. The comparison was carried out using: brain D2 and 5-HT2 receptor occupancy; animal models predictive of antipsychotic efficacy (amphetamine-induced hyperlocomotion (AIL) and conditioned avoidance response (CAR) models); measures predictive of side effects (catalepsy and prolactin elevation); and molecular markers predictive of antipsychotic action (striatal Fos induction). NDMC (10–60 mg/kg/s.c.) showed high 5-HT2 (64–79%), but minimal D2 occupancy (<15% at 60 mg/kg) 1 h after administration. In contrast to other antipsychotics, NDMC was not very effective in reducing AIL or CAR and showed minimal induction of Fos in the nucleus accumbens. However, like atypical antipsychotics, it showed no catalepsy, prolactin elevation, and minimal Fos in the dorsolateral striatum. It seems unlikely that NDMC would show efficacy as a stand-alone antipsychotic, however, its freedom from catalepsy and prolactin elevation, and its unique pharmacological profile (muscarinic agonism) may make it feasible to use this drug as an adjunctive treatment to existing antipsychotic regimens.
Similar content being viewed by others
INTRODUCTION
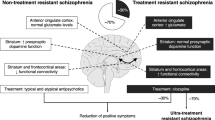
Despite its risk of causing agranulocytosis and seizures, clozapine still remains the gold-standard for efficacy in schizophrenia even after decades of new drug development (Kane et al, 1988; Buchanan, 1995; Volavka et al, 2002; Meltzer et al, 2003; Woodward et al, 2005). As compared to other antipsychotics, clozapine shows two unique abilities; a very low propensity for extrapyramidal symptoms (EPS) and efficacy in patients for whom other typical and atypical drugs have not been effective. There are several accounts for its freedom from EPS: low affinity for and low occupancy of D2 receptors, 5-HT2 antagonism, cholinergic effects, and 5-HT1A agonism (Meltzer et al, 1989; Farde et al, 1992; Rollema et al, 1997; Bymaster et al, 2003). However, the reason for its unique therapeutic efficacy is still not well understood. Recent clinical and preclinical data have raised the possibility of an important therapeutic role of clozapine's major metabolite N-desmethylclozapine (NDMC) (Sur et al, 2003; Weiner et al, 2004; Burstein et al, 2005; Davies et al, 2005; Li et al, 2005).
Clozapine undergoes extensive hepatic metabolism, of which NDMC and clozapine N-oxide are major metabolites (Pirmohamed et al, 1995; Dain et al, 1997). NDMC is formed by demethylation of clozapine by CYP1A2 and CYP3A4 isoforms of the P450-enzyme system (Eiermann et al, 1997; Olesen and Linnet, 2001), and across individuals there is significant variation in the metabolism of clozapine with levels ranging from 20 to 150% of the parent compound (Bondesson and Lindstrom, 1988; Perry et al, 1991). NDMC is reported to have a higher affinity to 5-HT2A, 5-HT2C, and muscarinic receptors (M1–M5) receptors, comparable affinity to D2 and lower affinity to D1 receptors (Kuoppamaki et al, 1993; Sur et al, 2003; Burstein et al, 2005) than the parent compound. At the muscarinic receptors, NDMC differs from clozapine by being a more potent partial agonist at M1 receptors and also shows increased agonist efficacy at M4 and M5 receptors (Weiner et al, 2004). The interest in a therapeutic role for NDMC has been highlighted by recent findings that high NDMC/clozapine ratios predict improvement in cognitive functioning and quality of life better than plasma levels of either compound alone (Weiner et al, 2004) though, not all previous studies have found positive benefits of a high NDMC/clozapine ratio (Dettling et al, 2000; Mauri et al, 2004). Also the recent identification of NDMC as a partial agonist at the D2 receptor has raised considerable interest in its possible role as an antipsychotic (Burstein et al, 2005) as aripiprazole, a recently introduced partial-agonist D2 antipsychotic, has been found to be effective, safe, and well tolerated for positive and negative symptoms in schizophrenia and schizoaffective disorder (Potkin et al, 2003).
In light of the growing interest in NDMC as a primary antipsychotic, we thought that it would be of particular relevance to compare the activity of NDMC to clozapine (its parent compound and an atypical D2 antagonist), haloperidol (an established typical agent), and aripiprazole (an established D2 partial agonist atypical antipsychotic) in models that have reliably predicted antipsychotic profiles in the past. The first question regarding NDMC was its ability to cross the blood–brain barrier, and so we began our investigations with dopamine D2 and 5-HT2 occupancy of NDMC and compared it to other antipsychotics. Next, we compared them in models of functional dopamine antagonism and antipsychotic efficacy: amphetamine-induced locomotor activity (AIL), conditioned avoidance response (CAR), and Fos induction in the nucleus accumbens (shell region), along with markers of motor side effects—catalepsy (CAT) and Fos expression in the dorsolateral striatum (Deutch et al, 1992; Robertson et al, 1994; Arnt and Skarsfeldt, 1998). Plasma prolactin levels, which serve as an endocrine marker of D2 receptor antagonism outside the blood–brain barrier, were also evaluated (Kapur et al, 2002).
MATERIALS AND METHODS
Animals
Adult male Sprague–Dawley rats weighing 250–275 g on arrival (Charles River Laboratories, Montreal, Canada), housed in pairs under reversed lighting conditions (12 h reverse light/dark cycle-lights off at 0800) and with access to food and water ad libitum were used. Animals were allowed to acclimatize to the housing facility for at least 5 days before being used for experimentation. All experiments were approved by the institute's animal care committee.
Drugs
Haloperidol (Sabex Inc., Boucherville, QC, Canada), clozapine (ANAWA Trading SA, Wangen, Zurich, Switzerland), aripiprazole (custom synthesized), and NDMC (a gift from ACADIA pharmaceuticals, San Diego, CA, USA) were used in the study. Aripiprazole was dissolved in 30% dimethylformamide (in physiological saline), whereas the other drugs were dissolved in 1–2% glacial acetic acid and made up to volume with physiological saline. d-Amphetamine sulphate was obtained from US Pharmacopoeia and dissolved in physiological saline. All drugs were administered subcutaneously (s.c.) in a volume of 1 ml/kg of body weight. [3H]raclopride and [3H]ketanserin (Perkin Elmer Life Sciences, Boston, MA, USA), used as radiotracers in the occupancy studies, were administered intravenously.
Occupancy and Catalepsy Experiments
Dose–response for D2/5-HT2 receptor occupancy (5-HT2RO) for haloperidol (0.025–1 mg/kg), clozapine (0.1–40 mg/kg), aripiprazole (0.3–30 mg/kg), and NDMC (3–60 mg/kg) were obtained by randomly assigning five animals to each dose level of drug testing. The animals received 7.5 μCi/rat of [3H]raclopride or [3H]ketanserin, diluted in saline in a constant volume of 0.4 ml, 30 or 45 min, respectively before killing (Sumiyoshi et al, 1995; Wadenberg et al, 2000b). Brain tissues (striatum or prefrontal cortex and cerebellum) were rapidly dissected and dissolved and counted using liquid scintillation spectrometry (Wadenberg et al, 2000b). Striatal, prefrontal, and cerebellar counts expressed as disintegrations per minute/mg (DPM/mg) of tissue were used for calculations. The ratio of striatum minus cerebellum (index of specific binding)/cerebellum (index of free and nonspecific binding) was used to obtain an index of the binding potential (BP) of dopamine D2 receptors and in case of 5-HT2 receptors, prefrontal cortex was used instead of striatal tissue (Farde et al, 1988; Kapur et al, 1999; Wadenberg et al, 2000b). The occupancy induced by the drug was calculated using the formula: %Occupancy=100 × (BPcontrols−BPdrug/BPcontrols); where BPcontrols is the pooled D2 or 5-HT2 binding potential of all the control animals and BPdrug is the D2 or 5-HT2 binding potential of a drug-treated animal. Occupancy curves and the ED50 values (dose at which 50% receptors are occupied) if attained were determined using the nonlinear regression equation representing a rectangular hyperbola, using Sigma Plot®. Catalepsy was evaluated in the same animals used for the occupancy experiment 10 min before killing. Animals were placed on an inclined grid (60°) and the time the animals remained immobile (excluding the first 30 s), was used as an index of catalepsy (on a scale 0–5) (Ahlenius and Hillegaart, 1986; Wadenberg et al, 2000b). An animal was considered cataleptic with a score greater than or equal to 2. Raters were blind to drug treatment and the ED50 values were evaluated using probit analysis (Finney, 1971).
Amphetamine-Induced Locomotion
The locomotor activity boxes were clear plexiglas housing cages, (27 × 48 × 20 cm) equipped with a row of six photocell beams placed 3 cm above the floor of the cage. A computer was used to detect and record the number of photobeam interruptions. For investigating the effects of haloperidol (0.01–0.5 mg/kg), clozapine (1–40 mg/kg), aripriprazole (0.3–10 mg/kg), and NDMC (10–100 mg/kg) on AIL, rats were first injected with the appropriate antipsychotic or vehicle and placed in the locomotor activity boxes for a period of 30 min. Then, d-amphetamine (1.5 mg/kg/s.c.) was administered and locomotor activity was monitored for a period of 60 min. The ED50 value was the dose that was required to inhibit 50% of locomotor activity counts recorded over the period of 60 min with respect to vehicle-treated amphetamine-administered animals and was calculated using nonlinear regression. Each group contained a minimum of six subjects at each dose level tested.
Conditioned Avoidance Responding
Rats were trained and tested in a computer assisted two-way active avoidance (shuttle boxes) apparatus (Med Associates, VT, USA) placed in a sound and light-attenuating ventilated chamber. The boxes were divided into two compartments of equal size with a microswitch detection system to identify the location and movement of the rat in the shuttle box from one compartment to the other. A 80 dB white-noise served as a conditioned stimulus which was followed 10 s later by a scrambled 0.8 mA shock as the unconditioned stimulus. Animals were habituated to the CAR boxes for 30 min before training and rats that moved to the other side of the box within the period of the conditioned stimulus only (10 s) were noted as having made an ‘avoidance’ response. Those who escaped the shock in the next 20 s were termed as having ‘escaped’, and those not escaping were termed as ‘escape failures’ (Wadenberg et al, 2001b). After 5 days of training, a performance criterion of greater than 80% avoidance served as the basis for selecting rats that were used for drug testing. The ED50 for CAR was the dose required to produce 50% inhibition of avoidance, and was calculated using probit analysis at the 90-min time point after drug administration (Finney, 1971). Haloperidol was tested at 0.01, 0.05, and 0.15 mg/kg in six subjects; clozapine was tested at doses of 5, 15, and 30 mg/kg in six subjects; aripiprazole was tested at 3, 10, and 30 mg/kg in six subjects; whereas NDMC was tested at 10, 30, and 100 mg/kg in six subjects. Animals of each drug group served as their own controls in a within-subject design. Animals were tested at 0, 20, 90, 240 min, and 24 h after drug administration with an interval of at least 2 days between experiments. The 0-min time point represents CAR testing before drug administration.
Fos Immunohistochemistry
Haloperidol (0.01–0.5 mg/kg), clozapine (7.5–50 mg/kg), aripiprazole (3–100 mg/kg), and NDMC (3–60 mg/kg) were evaluated. The animals were deeply anaesthetized with sodium pentobarbital (100 mg/kg i.p.), 2 h after drug administration and perfused transcardially with saline followed by 4% paraformaldehyde. The brains were removed, post-fixed in 4% paraformaldehyde, transferred to sucrose solutions (10% for 2 h, 20% for 12 h, and 30% for 24 h), and then dried and stored at −80°C until processing. Immunostaining was performed on free-floating, 40 μm cryostat sections with a polyclonal primary antiserum raised in rabbit against the Fos peptide (4–17 amino acids of human Fos; Oncogene Research Products, Cambridge, MA, USA), diluted 1 : 5000 and incubated for 48 h at 4°C. The tissue sections were then exposed to biotinylated goat anti-rabbit secondary antibody (1 : 200, Vector Laboratories, Burlingame, CA, USA), which was followed by incubation with horseradish peroxidase avidin–biotin complex (Vector Laboratories, Burlingame, CA, USA) to visualize the Fos staining. Fos-immunoreactive nuclei were counted within a 400 × 400 μm grid at a magnification of × 100 in the shell of the nucleus accumbens and dorsolateral striatum (bregma 1.70–1.00) (Paxinos and Watson, 1986; Robertson et al, 1994) using an MCID M5 imaging and software system (Imaging Research, St Catherines, ON, Canada). Cell counts were obtained from at least three separate brain sections for each brain, obtained from at least four subjects per group, by an observer who was blind to treatment conditions.
Plasma Prolactin Measurements
Prolactin levels were measured using plasma collected from rats killed for the occupancy experiment 1 h after drug administration. Plasma samples were stored in −80°C until they were assayed. The prolactin levels (ng/ml) were measured using a rat prolactin enzyme immunoassay kit (ALPCO Diagnostics®, Windham, NH, USA).
RESULTS
Occupancy
All drugs with the exception of NDMC showed dose-dependent striatal D2 receptor occupancy (D2RO) in the dose range tested 1 h after drug administration (Figure 1, Table 1). [3H] Raclopride resulted in an average binding potential of 6.08±2.42 (mean±SD) in the striatum in pooled control animals. Haloperidol in a dose range of 0.025–1 mg/kg showed a D2RO from 49 to 90% with an ED50 of 0.02 mg/kg (CI 95%: 0.02–0.03). In a dose range of 5–40 mg/kg clozapine showed D2RO from 28 to 62% with an ED50 of 15.48 mg/kg (CI 95%: 8.88–22.08). In the case of aripiprazole D2RO levels of 64–96% were achieved in a dose range of 0.3–30 mg/kg with an ED50 of 0.75(CI 95%: 0.55–0.95), NDMC on the other hand achieved a maximum of 13% D2RO at a dose of 60 mg/kg and in a dose range of 3–30 mg/kg its D2RO was less than 2% and hence its ED50 was not determined.
Striatal D2 receptor and prefrontal 5-HT2 occupancy (Mean±SD) 1 h after administration of haloperidol, clozapine, aripiprazole, and NDMC (n=5 for each dose level). Filled symbols in the occupancy graph represent cataleptic doses. The curves were generated using a nonlinear regression equation representing a rectangular hyperbola (y=ax/(b+x)) using Sigma Plot® software.
In the CAR experiment, NDMC at 100 mg/kg showed a statistically significant inhibition 240 min after treatment; unlike other antipsychotics, which were active within 1 h after drug administration. A separate study to look at the time course of D2RO occupancy of NDMC at two doses (30 and 100 mg/kg) was carried out, 240 and 360 min after drug administration. The dose of 30 mg/kg resulted in D2RO of 10.27 and 6.3% at 240 and 360 min post-drug administration, whereas 100 mg/kg resulted in D2RO of 42.92 and 37.8%, 240 and 360 min post-drug administration.
Clozapine and NDMC showed very high dose-dependent prefrontal 5-HT2RO whereas haloperidol and aripiprazole showed lower occupancy levels in the tested dose ranges 1 h after administration (Figure 1, Table 1). [3H] Ketanserin resulted in an average binding potential of 1.59±0.33 (mean±SD) in the prefrontal cortex in pooled control animals. The ED50 for haloperidol was 1 mg/kg (95%CI: 0.46–1.54) showing occupancy levels of 18–55% over a dose range of 0.1–1 mg/kg. Aripiprazole tested over a dose range of 1–30 mg/kg showed 5-HT2RO levels of 7–32% and its ED50 was not determined. Clozapine's 5-HT2RO ED50 was 0.19 mg/kg (95%CI: 0.09–0.29) and in a dose range of 0.1–40 mg/kg it showed occupancies ranging from 35 to 97%. NDMC in a dose range of 10–60 mg/kg showed 5-HT2RO from 64 to 79% with an ED50 of 6.6 mg/kg (95%CI: 2.56–15.76) extrapolated from the rectangular hyperbola (y=ax/(b+x)) used to fit the data. A separate study to look at the time course of 5-HT2RO occupancy of NDMC at 100 mg/kg was carried out, 240 min after drug administration, and it resulted in an occupancy of 98.14%.
Catalepsy
Doses of haloperidol (⩾0.1 mg/kg) that exceeded 80% D2RO showed CAT 1 h after drug treatment (Figure 1). None of the clozapine-treated animals showed CAT. In the case of aripiprazole none of the animals exhibited CAT even when the doses exceeded 90% D2RO. Also CAT was not observed in any of the animals administered with NDMC, tested 1 h as well as 4 and 6 h after drug administration.
Amphetamine-Induced Locomotion
Haloperidol, clozapine, and aripiprazole significantly inhibited AIL in a dose-dependent manner; however NDMC was only partially effective at a dose of 100 mg/kg 1 h after drug administration (Figure 2, Table 1). The ED50 for haloperidol was determined to be 0.027 mg/kg (CI 95%: 0.015–0.039), which corresponded to a D2RO of 53%. Clozapine's ED50 value in this assay was 4.16 mg/kg (CI 95%: 1.38–6.94) which was equivalent to 24% D2RO. Aripiprazole inhibited AIL with an ED50 value of 0.34 mg/kg (CI 95%: 0.24–0.44) and reflected a D2RO of 33%. NDMC was also tested in the AIL model 240 min post-treatment and showed a similar profile at that obtained 30 min post-treatment (Figure 2).
The effects of haloperidol, clozapine, aripiprazole, and NDMC (n=6) for each dose on locomotor activity measured for 1 h duration after amphetamine or saline administration and expressed as mean±SEM. The drugs or vehicle were administered 30 min or 4 h before amphetamine or saline challenge. **p<0.001, *p<0.05, one-way ANOVA F(19,80)=18.93; post hoc Dunnett (two sided) with respect to pooled amphetamine treatment.
CAR
All the standard drugs inhibited CAR significantly at the tested doses (Figure 3, Table 1). Haloperidol showed a significant reduction in CAR 20 min after drug administration and its ED50 90 min post-treatment was determined to be 0.03 mg/kg (95%CI: 0.004–0.06) and correlated to a D2RO of 51%. Clozapine treatment also resulted in a significant reduction in CAR 20 min after drug administration and its ED50 (90 min) was determined to be 7.77 mg/kg (95%CI: 2.34–15.11), which corresponded to a D2RO of 36%. Aripiprazole's ED50 90 min post-drug administration was determined to be 5.85 mg/kg (95% CI: 2.62–10.98) which was equivalent to 82% D2RO. There were no escape failures throughout the trials and all drug-treated animals returned to their baseline 24 h after drug administration.
Effect of haloperidol (n=6), clozapine (n=6), aripiprazole (n=6), and NDMC (n=6) on the performance of CAR in rats after single s.c. injection. The animals served as their own controls using a within-subject design. Values of percentage inhibition of avoidance are expressed as mean±SEM. The avoidance values were analyzed for each drug in a repeated measures ANOVA with dose (vehicle, three drug doses) as a within-subject factor for each time point separately. If the sphericity assumption was not met Huynh–Feldt correction was applied and the main effect of dose was significant at least at one time point for all the drugs. Post hoc comparisons were performed using the Bonferroni adjustment for multiple comparisons and the level of significance indicated in the figure is that with respect to vehicle treatment (*p<0.05).
NDMC did not inhibit CAR up to a dose of 30 mg/kg at any time point—either at 20, 90, 240 min, or 24 h after dosing. The dose of 100 mg/kg did inhibit CAR, but only at 240 min after drug administration, an effect not seen with any of the lower doses. In comparison to other antipsychotics the ED50 value at the 90 min for NDMC would exceed 100 mg/kg. The maximal inhibition of CAR by NDMC at the 240-min time point was 75% at a dose of 100 mg/kg (corresponding to a D2RO of 42.92%) and lower doses were not effective. There were no escape failures throughout the trials and all drug-treated animals returned to their baseline 24 h after drug administration.
Fos Expression
Induction of Fos was measured over different doses in the nucleus accumbens as well as the dorsolateral striatum for all the four drugs (Figure 4). For haloperidol significant Fos induction in the nucleus accumbens (shell) emerged when occupancies exceeded 60% D2RO. The lowest dose of clozapine that was tested (7.5 mg/kg–35% D2RO) showed significant Fos induction in the nucleus accumbens. Doses of aripiprazole <70%D2RO (3 mg/kg) occupancy, did not produce a discernable Fos signal in the accumbens, and Fos became observable only at occupancies exceeding 80% D2RO (10 mg/kg) (Figure 4). Only the highest dose of NDMC (60 mg/kg∼13% D2RO) tested showed statistically significant Fos induction (Figure 5).
Fos expression in the nucleus accumbens and dorsolateral striatum owing to drug treatment (n=4 for each dose). Rats were killed 2 h after drug administration and Fos immunoreactive nuclei expressed as mean±SEM was counted within a 400 × 400 μm grid in the specified brain regions. **p<0.001, *p<0.05, one-way ANOVA F(16,67)=23.93; post hoc Dunnett (two sided) with respect to pooled vehicle control of nucleus accumbens. †p<0.05, one-way ANOVA F(16,67)=19.01; post hoc Dunnett (two sided) with respect to pooled vehicle treatment of dorsolateral striatum.
Haloperidol at the dose of 0.5 mg/kg that has the propensity for inducing CAT (D2RO >80%) clearly showed high levels of Fos induction in the dorsolateral striatum (greater than 30 counts in a 400 × 400 μm area). Although there was a statistically significant increase in Fos expression in the dorsolateral striatum at higher doses of aripiprazole (D2RO >80%), the extent of Fos expression did not translate into motor side effects as evaluated by CAT (Figure 4). Clozapine and NDMC in the dose range tested did not significantly induce Fos in the dorsolateral striatum correlating with their lack of CAT (Figure 5).
Prolactin
Haloperidol showed a dose-related prolactin induction 1 h after drug administration (Figure 6). In the haloperidol group one rat in the 0.05 mg/kg treatment group was a significant outlier (prolactin value of 140 ng/ml; Grubbs test Z=1.71, p<0.05) and was excluded from the calculations and one sample in the 1 mg/kg group was lost owing to contamination. In the case of aripiprazole, at the dose of 10 mg/kg, a small increase was obtained and higher doses did not show any statistically significant elevation of prolactin levels. Clozapine and NDMC did not cause increase in prolactin induction 1 h after drug administration at the doses tested. Haloperidol at a dose of 0.05 mg/kg where significant elevation of prolactin is observed corresponds to >60%D2RO whereas aripiprazole did not show prolactin elevation at D2RO >90% (30 mg/kg). Prolactin levels tested for NDMC 240 and 360 min after drug administration for 30 and 100 mg/kg were not significant from the vehicle controls (one-way analysis of variance (ANOVA) F(4,25)=0.74; post hoc Dunnett (two sided) with respect to pooled vehicle control).
Plasma prolactin levels after haloperidol, clozapine, aripiprazole, and NDMC treatment measured from plasma samples obtained from the occupancy experiment 1 h after s.c. administration (minimum of n=4 for each dose). Values are expressed as mean±SEM, *p<0.005, one-way ANOVA F(16,86)=13.25; post hoc Dunnett (two sided) with respect to the pooled vehicle control.
DISCUSSION
We began by assessing NDMC's ability to enter the brain, especially given the conflicting data available on NDMC's brain levels as a metabolite during clozapine treatment in rodents (Baldessarini et al, 1993; Weigmann et al, 1999). Clearly, NDMC 1 h after drug administration, showed an orderly and dose-dependent occupancy of 5-HT2 receptors however, its occupancy of D2 receptors was rather low. The results clearly demonstrate that despite NDMC's ability to enter the brain, its D2RO is low. Clozapine's in vitro affinity ratio D2(20 nM)/5-HT2 (5 nM) is 4 and that for NDMC D2(63 nM)/5-HT2(5 nM) is 12.6 (Weiner et al, 2004). Clozapine's in vivo ED50 ratio D2(15.48 mg/kg)/5-HT2(0.19 mg/kg) is 81 and if a similar ratio is applicable to NDMC (given its structural similarity to clozapine and an ED50 value of 6.6 mg/kg for 5-HT2RO) the ED50 for D2 in vivo occupancy would exceed 500 mg/kg. The lower affinity to D2 receptors compared to 5-HT2 receptors partially explains NDMC's lack of significant occupancy at the D2 receptors, 1 h after administration.
The low D2RO of NDMC is consistent with its lack of catalepsy or prolactin elevation, as these measures have been closely linked to D2RO for other agents (Wadenberg et al, 2000b; Natesan et al, 2006). In the AIL model, NDMC had the least effects among the established antipsychotics tested. Clozapine's ED50 for the AIL model is 4.16 mg/kg and it occupies 25% D2 receptors at that dose. NDMC achieves this level of occupancy at a very high dose (100 mg/kg) and at time points much later (43%, 240-min post-drug administration) than that of clozapine. In the case of other D2 antagonists/partial agonists, inhibition of AIL (ED50) is seen at striatal D2 occupancies ∼50–60% (Natesan et al, 2006). However, in the case of NDMC this level of occupancy is not achieved even at the high dose of 100 mg/kg observed up to 360-min post-treatment. 5-HT2 receptor antagonism (O’Neill et al, 1999) and muscarinic M1 agonism (Bymaster et al, 1999) are known to inhibit AIL and it is likely that they could have influenced inhibition of AIL, although at a very high dose.
The CAR model has very high predictive validity for antipsychotic efficacy, and this relationship is driven not only by drug effects on D2 receptors, but, is also influenced by dopamine D1 (McQuade et al, 1992), adrenergic (Hertel et al, 1999; Wadenberg et al, 2000a; Linner et al, 2002), glutaminergic (Takamori et al, 2003), muscarinic (Shannon et al, 1999), and serotonergic (Wadenberg et al, 1994, 2001a) receptor systems. NDMC was ineffective at the 20–90-min time point where all the other effective antipsychotics demonstrate efficacy. NDMC was effective 240 min after drug administration, and that only at a dose of 100 mg/kg where its D2RO was 43%. The reason for such late emergence does not seem to be slower brain penetration of NDMC as it occupies 5-HT2 receptors at a much earlier time point. It is plausible that NDMC is probably being converted to a metabolite (or back-converted to clozapine) (Chang et al, 1998) and it is these latter agents that are responsible for its late-appearing efficacy. Regardless of which moiety is most active at the time period—one plausible mechanism for this late appearing action is its modest levels of D2 occupancy at that time period. It is possible that NDMC may act like an antagonist because of its low level of intrinsic activity on D2 receptors, and given its comparable level of D2 occupancy (43% at 100 mg/kg) with that of clozapine at effective doses (CAR ED50 36%), the effects in CAR may be due to D2 receptor antagonism. It has also been suggested that NDMC has muscarinic agonist action (Sur et al, 2003) and muscarinic agonism has been shown to independently have an effect on CAR (Shannon et al, 1999). Though we could not measure muscarinic agonist effects of this agent, it is plausible that its muscarinic effects when combined with its modest D2 occupancy lead to the late-emerging inhibition of CAR at a high dose.
Drug-induced patterns of expression of the immediate early gene c-Fos (first signs of a genomic response) are useful mapping tools for regions of activation of different drug classes acting on the central nervous system (Herrera and Robertson, 1996; Sumner et al, 2004). Fos protein expression in the nucleus accumbens (shell) is common to all clinically effective antipsychotic drugs whereas increases in Fos expression in the caudate putamen (dorsolateral striatum) are associated with motor side effects (Deutch et al, 1992; Robertson et al, 1994). NDMC induced Fos in the nucleus accumbens (shell) only at a high dose of 60 mg/kg and even at those doses expression in the dorsolateral striatum was not significant. This study replicates the findings of Young et al (1998) wherein increased Fos protein expression in the medial prefrontal cortex and nucleus accumbens was observed, but not in the dorsolateral striatum. However, in the present study Fos expression of comparators, haloperidol, clozapine, and aripiprazole in the nucleus accumbens (shell), correlates well with the presence/absence of CAR inhibition at a certain threshold of Fos expression (the doses at which these drugs inhibited CAR were usually related to >20 counts in a 400 × 400 μm area). The Fos expression induced by a dose of 60 mg/kg for NDMC does not exceed this threshold and could explain the lack of effect in CAR at early time points. The emergence of catalepsy is correlated with a certain threshold of Fos expression (>30 counts) in the dorsolateral striatum among antipsychotic agents (Natesan et al, 2006). In the present study, only haloperidol exceeded this level of Fos expression, and showed catalepsy. Clozapine, aripiprazole, and NDMC showed limited levels Fos expression in this region even at the highest tested doses. As, in the case of clozapine and aripiprazole this has meant freedom from EPS clinically, it is likely that NDMC too will show freedom from motor side effects even at high doses. Clozapine's lack of prolactin elevation might be due to its low affinity. NDMC also has low affinity to the D2 receptor, and at the same time is a partial agonist. These two qualities may explain why we did not observe prolactin elevation.
At present there are no clinical studies of NDMC by itself. All inferences about NDMC's clinical potential are derived from studies of clozapine by measuring the plasma levels of NDMC or the ratio of NDMC/clozapine in these patients. It has been claimed that NDMC may derive unique efficacy via its muscarinic receptor agonist properties, and furthermore that clozapine's unique efficacy in clinically refractory patients may be a function of its conversion to NDMC (Weiner et al, 2004). As clozapine is a cholinergic antagonist (Bolden et al, 1991) and NDMC is claimed to be a cholinergic agonist, the overall effects when NDMC is generated in a patient on clozapine would depend on the ratio of NDMC to clozapine. It has been suggested that patients who have a higher ratio of NDMC/clozapine may provide an indirect glimpse of the possible unique contributions of NDMC. In a recent study by Weiner et al (2004) showed that higher NDMC/clozapine ratios predicted greater improvement in subscales of quality of life measures, multiple measures of cognition as well as in some subscales of negative symptomatology and also predicted improvement in delusions, but not hallucinations. However, not everyone finds a positive impact of higher NDMC/clozapine—even this measure has met with conflicting findings in terms of clinical response to clozapine treatment ranging from no correlation (Dettling et al, 2000; Mauri et al, 2004) to a positive one (Hasegawa et al, 1993; Spina et al, 2000; Frazier et al, 2003; Mauri et al, 2003; Weiner et al, 2004). Thus, while one can only draw indirect inferences from mixed NDMC/clozapine studies, there are some hints that NDMC may be contributing additional anti ‘psychotic’ or pro-cognitive efficacy via its muscarinic effects.
In addition to its in vitro evidence for muscarinic agonism, in vivo evidence comes from the fact that in rodents NDMC administration, but not clozapine, leads to a dose-dependent activation of mitogen-activated protein kinase (MAPK) in the CA1 region of the hippocampus and also potentiates NDMA receptor currents, actions mediated by the muscarinic M1 receptors (Berkeley et al, 2001; Sur et al, 2003; Weiner et al, 2004). In fact muscarinic agonists like xanomeline, BuTAC, and PTAC (which are relatively devoid of D2 activity) have been shown to be very active in CAR (Bymaster et al, 1999, 2002) and xanomeline has been shown to have antipsychotic and pro-cognitive efficacy in humans (Bodick et al, 1997). However in the case of NDMC, in the dose range tested, it did not effectively inhibit CAR at the 20–90-min time point where other M1 agonists/partial agonists have inhibited CAR significantly after s.c. administration (Shannon et al, 1999). It is possible that either NDMC did not reach sufficient receptor occupancies of muscarinic receptors, or the level of its intrinsic activity at the muscarinic receptor subtypes was too low to inhibit CAR. The animal models used in the present study mostly reflect efficacy against positive symptoms in schizophrenia and we did not have any test in our battery that readily addresses the claim of cognitive enhancement by NDMC (Floresco et al, 2005).
In summary, the results of this study especially against the backdrop of very consistent findings with established antipsychotics suggests that NDMC will be an effective antipsychotic, if at all, only at very high doses in humans. The fact that NDMC did not induce any motor side effects, Fos expression in the dorsolateral striatum, or prolactin elevation at very high doses suggests that it will be free from the conventional side effects associated with antipsychotics. This keeps open the feasibility of NDMC being used as an adjunct to enhance efficacy of other antipsychotics especially in refractory patients—a hypothesis that could be tested in humans.
References
Ahlenius S, Hillegaart V (1986). Involvement of extrapyramidal motor mechanisms in the suppression of locomotor activity by antipsychotic drugs: a comparison between the effects produced by pre- and post-synaptic inhibition of dopaminergic neurotransmission. Pharmacol Biochem Behav 24: 1409–1415.
Arnt J, Skarsfeldt T (1998). Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacology 18: 63–101.
Baldessarini RJ, Centorrino F, Flood JG, Volpicelli SA, Huston-Lyons D, Cohen BM (1993). Tissue concentrations of clozapine and its metabolites in the rat. Neuropsychopharmacology 9: 117–124.
Berkeley JL, Gomeza J, Wess J, Hamilton SE, Nathanson NM, Levey AI (2001). M1 muscarinic acetylcholine receptors activate extracellular signal-regulated kinase in CA1 pyramidal neurons in mouse hippocampal slices. Mol Cell Neurosci 18: 512–524.
Bodick NC, Offen WW, Levey AI, Cutler NR, Gauthier SG, Satlin A et al (1997). Effects of xanomeline, a selective muscarinic receptor agonist, on cognitive function and behavioral symptoms in Alzheimer disease. Arch Neurol 54: 465–473.
Bolden C, Cusack B, Richelson E (1991). Clozapine is a potent and selective muscarinic antagonist at the five cloned human muscarinic acetylcholine receptors expressed in CHO-K1 cells. Eur J Pharmacol 192: 205–206.
Bondesson U, Lindstrom LH (1988). Determination of clozapine and its N-demethylated metabolite in plasma by use of gas chromatography-mass spectrometry with single ion detection. Psychopharmacology (Berlin) 95: 472–475.
Buchanan RW (1995). Clozapine: efficacy and safety. Schizophr Bull 21: 579–591.
Burstein ES, Ma J, Wong S, Gao Y, Pham E, Knapp AE et al (2005). Intrinsic efficacy of antipsychotics at human D2, D3, and D4 dopamine receptors: identification of the clozapine metabolite N-desmethylclozapine as a D2/D3 partial agonist. J Pharmacol Exp Ther 315: 1278–1287.
Bymaster FP, Felder C, Ahmed S, McKinzie D (2002). Muscarinic receptors as a target for drugs treating schizophrenia. Curr Drug Targets CNS Neurol Disord 1: 163–181.
Bymaster FP, Felder CC, Tzavara E, Nomikos GG, Calligaro DO, McKinzie DL (2003). Muscarinic mechanisms of antipsychotic atypicality. Prog Neuropsychopharmacol Biol Psychiatry 27: 1125–1143.
Bymaster FP, Shannon HE, Rasmussen K, DeLapp NW, Ward JS, Calligaro DO et al (1999). Potential role of muscarinic receptors in schizophrenia. Life Sci 64: 527–534.
Chang WH, Lin SK, Lane HY, Wei FC, Hu WH, Lam YW et al (1998). Reversible metabolism of clozapine and clozapine N-oxide in schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry 22: 723–739.
Dain JG, Nicoletti J, Ballard F (1997). Biotransformation of clozapine in humans. Drug Metab Dispos 25: 603–609.
Davies MA, Compton-Toth BA, Hufeisen SJ, Meltzer HY, Roth BL (2005). The highly efficacious actions of N-desmethylclozapine at muscarinic receptors are unique and not a common property of either typical or atypical antipsychotic drugs: is M1 agonism a pre-requisite for mimicking clozapine's actions? Psychopharmacology (Berlin) 178: 451–460.
Dettling M, Sachse C, Brockmoller J, Schley J, Muller-Oerlinghausen B, Pickersgill I et al (2000). Long-term therapeutic drug monitoring of clozapine and metabolites in psychiatric in- and outpatients. Psychopharmacology (Berlin) 152: 80–86.
Deutch AY, Lee MC, Iadarola MJ (1992). Regionally specific effects of atypical antipsychotic drugs on striatal Fos expression: the nucleus accumbens shell as a locus of antipsychotic action. Mol Cell Neuroscience 3: 332–341.
Eiermann B, Engel G, Johansson I, Zanger UM, Bertilsson L (1997). The involvement of CYP1A2 and CYP3A4 in the metabolism of clozapine. Br J Clin Pharmacol 44: 439–446.
Farde L, Nordstrom AL, Wiesel FA, Pauli S, Halldin C, Sedvall G (1992). Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry 49: 538–544.
Farde L, Wiesel FA, Halldin C, Sedvall G (1988). Central D2-dopamine receptor occupancy in schizophrenic patients treated with antipsychotic drugs. Arch Gen Psychiatry 45: 71–76.
Finney DJ (1971). Probit Analysis. Cambridge University Press: London.
Floresco SB, Geyer MA, Gold LH, Grace AA (2005). Developing predictive animal models and establishing a preclinical trials network for assessing treatment effects on cognition in schizophrenia. Schizophr Bull 31: 888–894.
Frazier JA, Cohen LG, Jacobsen L, Grothe D, Flood J, Baldessarini RJ et al (2003). Clozapine pharmacokinetics in children and adolescents with childhood-onset schizophrenia. J Clin Psychopharmacol 23: 87–91.
Hasegawa M, Gutierrez-Esteinou R, Way L, Meltzer HY (1993). Relationship between clinical efficacy and clozapine concentrations in plasma in schizophrenia: effect of smoking. J Clin Psychopharmacol 13: 383–390.
Herrera DG, Robertson HA (1996). Activation of c-fos in the brain. Prog Neurobiol 50: 83–107.
Hertel P, Fagerquist MV, Svensson TH (1999). Enhanced cortical dopamine output and antipsychotic-like effects of raclopride by alpha2 adrenoceptor blockade. Science 286: 105–107.
Kane J, Honigfeld G, Singer J, Meltzer H (1988). Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45: 789–796.
Kapur S, Langlois X, Vinken P, Megens AA, De Coster R, Andrews JS (2002). The differential effects of atypical antipsychotics on prolactin elevation are explained by their differential blood–brain disposition: a pharmacological analysis in rats. J Pharmacol Exp Ther 302: 1129–1134.
Kapur S, Zipursky RB, Remington G (1999). Clinical and theoretical implications of 5-HT2 and D2 receptor occupancy of clozapine, risperidone, and olanzapine in schizophrenia. Am J Psychiatry 156: 286–293.
Kuoppamaki M, Syvalahti E, Hietala J (1993). Clozapine and N-desmethylclozapine are potent 5-HT1C receptor antagonists. Eur J Pharmacol 245: 179–182.
Li Z, Huang M, Ichikawa J, Dai J, Meltzer HY (2005). N-desmethylclozapine, a major metabolite of clozapine, increases cortical acetylcholine and dopamine release in vivo via stimulation of M1 muscarinic receptors. Neuropsychopharmacology 30: 1986–1995.
Linner L, Wiker C, Wadenberg ML, Schalling M, Svensson TH (2002). Noradrenaline reuptake inhibition enhances the antipsychotic-like effect of raclopride and potentiates D2-blockage-induced dopamine release in the medial prefrontal cortex of the rat. Neuropsychopharmacology 27: 691–698.
Mauri M, Volonteri LS, Fiorentini A, Invernizzi G, Nerini T, Baldi M et al (2004). Clinical outcome and plasma levels of clozapine and norclozapine in drug-resistant schizophrenic patients. Schizophr Res 66: 197–198.
Mauri MC, Volonteri LS, Dell’Osso B, Regispani F, Papa P, Baldi M et al (2003). Predictors of clinical outcome in schizophrenic patients responding to clozapine. J Clin Psychopharmacol 23: 660–664.
Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A et al (2003). Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 60: 82–91.
Meltzer HY, Matsubara S, Lee JC (1989). The ratios of serotonin2 and dopamine2 affinities differentiate atypical and typical antipsychotic drugs. Psychopharmacol Bull 25: 390–392.
McQuade RD, Duffy RA, Coffin VL, Barnett A (1992). In vivo binding to dopamine receptors: a correlate of potential antipsychotic activity. Eur J Pharmacol 251: 29–34.
Natesan S, Reckless GE, Nobrega JN, Fletcher PJ, Kapur S (2006). Dissociation between in vivo occupancy and functional antagonism of dopamine D(2) receptors: comparing aripiprazole to other antipsychotics in animal models. Neuropsychopharmacology 31: 1854–1863.
Olesen OV, Linnet K (2001). Contributions of five human cytochrome P450 isoforms to the N-demethylation of clozapine in vitro at low and high concentrations. J Clin Pharmacol 41: 823–832.
O’Neill MF, Heron-Maxwell CL, Shaw G (1999). 5-HT2 receptor antagonism reduces hyperactivity induced by amphetamine, cocaine, and MK-801 but not D1 agonist C-APB. Pharmacol Biochem Behav 63: 237–243.
Paxinos G, Watson C (1986). The Rat Brain in Stereotaxic Coordinates. Academic press: New York.
Perry PJ, Miller DD, Arndt SV, Cadoret RJ (1991). Clozapine and norclozapine plasma concentrations and clinical response of treatment-refractory schizophrenic patients. Am J Psychiatry 148: 231–235.
Pirmohamed M, Williams D, Madden S, Templeton E, Park BK (1995). Metabolism and bioactivation of clozapine by human liver in vitro. J Pharmacol Exp Ther 272: 984–990.
Potkin SG, Saha AR, Kujawa MJ, Carson WH, Ali M, Stock E et al (2003). Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry 60: 681–690.
Robertson GS, Matsumura H, Fibiger HC (1994). Induction patterns of Fos-like immunoreactivity in the forebrain as predictors of atypical antipsychotic activity. J Pharmacol Exp Ther 271: 1058–1066.
Rollema H, Lu Y, Schmidt AW, Zorn SH (1997). Clozapine increases dopamine release in prefrontal cortex by 5-HT1A receptor activation. Eur J Pharmacol 338: R3–R5.
Shannon HE, Hart JC, Bymaster FP, Calligaro DO, DeLapp NW, Mitch CH et al (1999). Muscarinic receptor agonists, like dopamine receptor antagonist antipsychotics, inhibit conditioned avoidance response in rats. J Pharmacol Exp Ther 290: 901–907.
Spina E, Avenoso A, Salemi M, Facciola G, Scordo MG, Ancione M et al (2000). Plasma concentrations of clozapine and its major metabolites during combined treatment with paroxetine or sertraline. Pharmacopsychiatry 33: 213–217.
Sumiyoshi T, Suzuki K, Sakamoto H, Yamaguchi N, Mori H, Shiba K et al (1995). Atypicality of several antipsychotics on the basis of in vivo dopamine-D2 and serotonin-5HT2 receptor occupancy. Neuropsychopharmacology 12: 57–64.
Sumner BE, Cruise LA, Slattery DA, Hill DR, Shahid M, Henry B (2004). Testing the validity of c-fos expression profiling to aid the therapeutic classification of psychoactive drugs. Psychopharmacology (Berlin) 171: 306–321.
Sur C, Mallorga PJ, Wittmann M, Jacobson MA, Pascarella D, Williams JB et al (2003). N-desmethylclozapine, an allosteric agonist at muscarinic 1 receptor, potentiates N-methyl-D-aspartate receptor activity. Proc Natl Acad Sci USA 100: 13674–13679.
Takamori K, Hirota S, Chaki S, Tanaka M (2003). Antipsychotic action of selective group II metabotropic glutamate receptor agonist MGS0008 and MGS0028 on conditioned avoidance responses in the rat. Life Sci 73: 1721–1728.
Volavka J, Czobor P, Sheitman B, Lindenmayer JP, Citrome L, McEvoy JP et al (2002). Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry 159: 255–262.
Wadenberg MG, Browning JL, Young KA, Hicks PB (2001a). Antagonism at 5-HT(2A) receptors potentiates the effect of haloperidol in a conditioned avoidance response task in rats. Pharmacol Biochem Behav 68: 363–370.
Wadenberg ML, Cortizo L, Ahlenius S (1994). Evidence for specific interactions between 5-HT1A and dopamine D2 receptor mechanisms in the mediation of extrapyramidal motor functions in the rat. Pharmacol Biochem Behav 47: 509–513.
Wadenberg ML, Hertel P, Fernholm R, Hygge Blakeman K, Ahlenius S, Svensson TH (2000a). Enhancement of antipsychotic-like effects by combined treatment with the alpha1-adrenoceptor antagonist prazosin and the dopamine D2 receptor antagonist raclopride in rats. J Neural Transm 107: 1229–1238.
Wadenberg ML, Kapur S, Soliman A, Jones C, Vaccarino F (2000b). Dopamine D2 receptor occupancy predicts catalepsy and the suppression of conditioned avoidance response behavior in rats. Psychopharmacology (Berlin) 150: 422–429.
Wadenberg ML, Soliman A, VanderSpek SC, Kapur S (2001b). Dopamine D(2) receptor occupancy is a common mechanism underlying animal models of antipsychotics and their clinical effects. Neuropsychopharmacology 25: 633–641.
Weigmann H, Hartter S, Fischer V, Dahmen N, Hiemke C (1999). Distribution of clozapine and desmethylclozapine between blood and brain in rats. Eur Neuropsychopharmacol 9: 253–256.
Weiner DM, Meltzer HY, Veinbergs I, Donohue EM, Spalding TA, Smith TT et al (2004). The role of M1 muscarinic receptor agonism of N-desmethylclozapine in the unique clinical effects of clozapine. Psychopharmacology (Berlin) 177: 207–216.
Woodward ND, Purdon SE, Meltzer HY, Zald DH (2005). A meta-analysis of neuropsychological change to clozapine, olanzapine, quetiapine, and risperidone in schizophrenia. Int J Neuropsychopharmacol 8: 457–472.
Young CD, Meltzer HY, Deutch AY (1998). Effects of desmethylclozapine on Fos protein expression in the forebrain: in vivo biological activity of the clozapine metabolite. Neuropsychopharmacology 19: 99–103.
Acknowledgements
We thank ACADIA pharmaceuticals, San Diego, CA, USA for the supply of NDMC. Jun Parkes of the PET group of CAMH is acknowledged for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Natesan, S., Reckless, G., Barlow, K. et al. Evaluation of N-Desmethylclozapine as a Potential Antipsychotic—Preclinical Studies. Neuropsychopharmacol 32, 1540–1549 (2007). https://doi.org/10.1038/sj.npp.1301279
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301279
Keywords
This article is cited by
-
Sex-dependent effects of long-term clozapine or haloperidol medication on red blood cells and liver iron metabolism in Sprague Dawley rats as a model of metabolic syndrome
BMC Pharmacology and Toxicology (2022)
-
Muscarinic and Nicotinic Acetylcholine Receptor Agonists and Allosteric Modulators for the Treatment of Schizophrenia
Neuropsychopharmacology (2012)
-
Involvement of histamine receptors in the atypical antipsychotic profile of clozapine: a reassessment in vitro and in vivo
Psychopharmacology (2012)
-
Further characterization of the discriminative stimulus properties of the atypical antipsychotic drug clozapine in C57BL/6 mice: role of 5-HT2A serotonergic and α1 adrenergic antagonism
Psychopharmacology (2009)
-
Better pharmacotherapy for schizophrenia: What does the future hold?
Current Psychiatry Reports (2008)